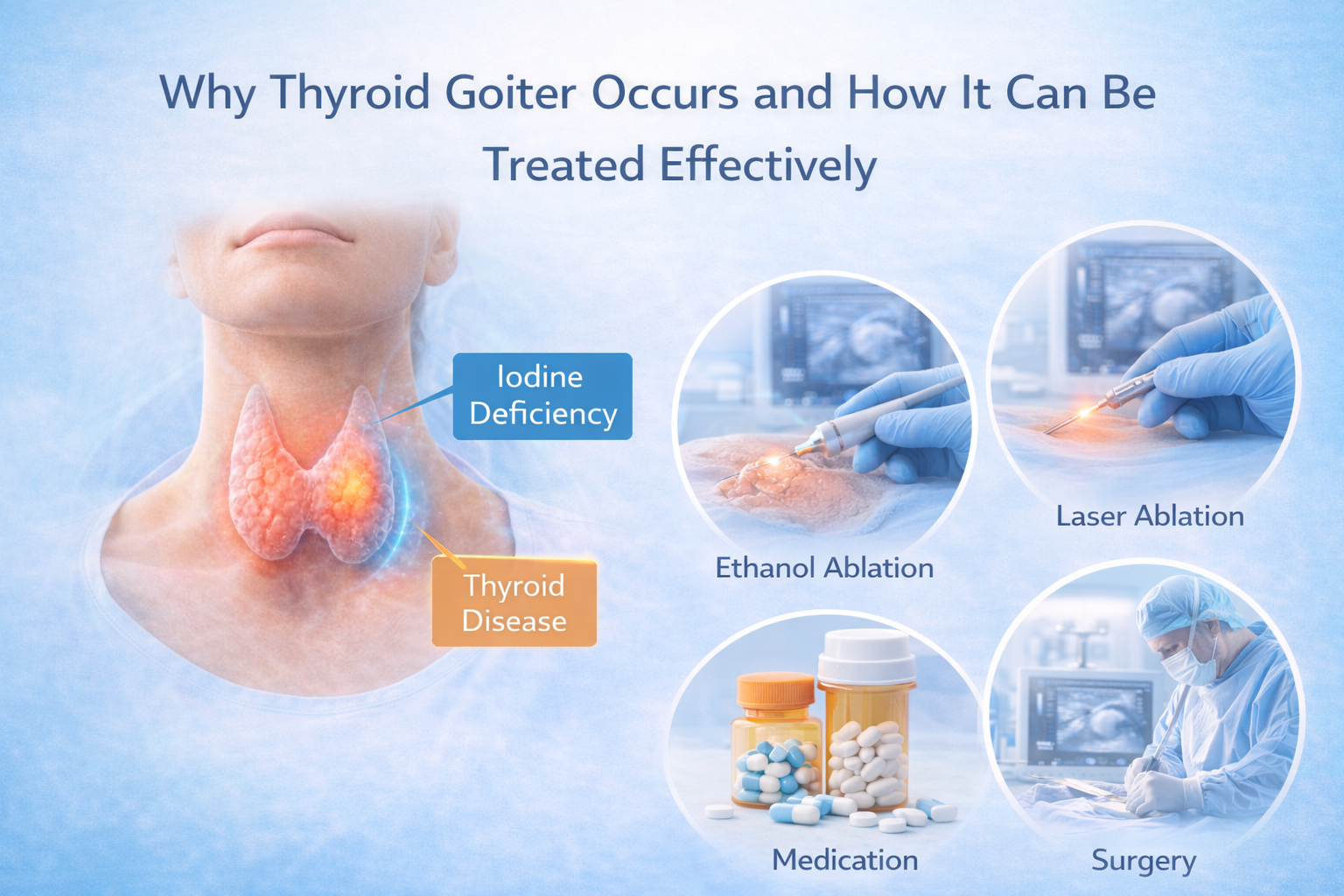
Thyroid goiter occurs when the thyroid gland enlarges due to hormonal imbalance, iodine deficiency, structural changes, or autoimmune activity, and the appropriate treatment depends on the underlying cause. A goiter itself is not a disease but a physical sign indicating that the thyroid is under stress. Many goiters remain benign and manageable without surgery, while others require medical, minimally invasive, or surgical intervention. Understanding both why thyroid goiter occurs and the available treatment options helps patients take timely action, prevent complications, and select the most appropriate management plan for their condition.
Hormonal Imbalance: A Leading Cause of Thyroid Goiter
Thyroid goiter frequently develops when thyroid hormone levels are abnormal. Low hormone levels trigger the pituitary gland to release excess thyroid-stimulating hormone (TSH), which repeatedly stimulates the thyroid gland to grow in order to produce more hormones. Over time, this chronic stimulation leads to an enlarged gland, sometimes visible as swelling in the neck.
In contrast, some forms of goiter are caused by excessive hormone production, where the thyroid enlarges in response to abnormal internal signals. Hormonal imbalance explains why goiter often accompanies hypothyroidism or hyperthyroidism. Patients experiencing fatigue, weight changes, or neck swelling should get their hormone levels tested, as early detection and treatment can prevent further enlargement.
Iodine Deficiency as a Trigger for Goiter
Iodine is a critical nutrient for producing thyroid hormones. When iodine intake is insufficient, the thyroid cannot synthesize adequate hormones, prompting the body to compensate by stimulating the gland to grow. This chronic stimulation results in goiter formation.
While iodine deficiency is less common in developed countries due to fortified salt and food, it still occurs in certain populations due to dietary restrictions, absorption issues, or specific medical conditions. Supplementing iodine under medical supervision can halt progression, and in mild cases, may reduce the size of the goiter without invasive procedures.
Structural Thyroid Changes and Nodules Causing Goiter
Some thyroid goiters develop because of structural changes in the gland, including benign nodules or cysts. These nodules can grow independently of hormone levels, causing uneven enlargement of the thyroid. Multiple nodules can lead to multinodular goiter, creating noticeable swelling in the neck and sometimes producing pressure on surrounding structures, such as the windpipe or esophagus.
Even if blood tests are normal, structural goiters can grow over time. Imaging, such as ultrasound or CT scans, is essential to monitor nodules, assess risk, and decide whether non-surgical treatments like Thyroid Nodule Ablation (RFA) or surgery are needed. Understanding the structural component helps physicians choose the safest and most effective treatment.
Autoimmune Thyroid Disorders Leading to Goiter
Autoimmune thyroid disorders, including Hashimoto’s thyroiditis and Graves’ disease, are major contributors to goiter formation. In these conditions, the immune system mistakenly attacks thyroid tissue, leading to inflammation, fibrosis, and abnormal hormone production.
Chronic autoimmune activity results in progressive gland enlargement, which can fluctuate in size depending on the disease’s activity. Patients with autoimmune-related goiters may experience fatigue, swelling, palpitations, or changes in body temperature. Long-term medical management, monitoring, and sometimes non-surgical interventions are essential to manage the gland effectively and prevent complications.
Effective Medical Management for Thyroid Goiter
Treatment for thyroid goiter depends on the cause, size, and symptoms. Medication is often the first-line therapy, particularly for hormonal or iodine-related causes.
- Thyroid hormone therapy can normalize hormone levels and reduce gland stimulation, which helps prevent further enlargement.
- Anti-thyroid medications are prescribed for hyperthyroid-related goiter, controlling hormone overproduction.
- Iodine supplementation is recommended for goiters caused by deficiency, helping to restore normal hormone synthesis.
These medical treatments aim to stabilize thyroid function, prevent further growth, and, in some cases, shrink the goiter over time. Regular follow-ups are necessary to monitor progress and adjust therapy as needed.
Minimally Invasive Non-Surgical Treatment Options
For patients whose goiters persist or cause discomfort, non-surgical procedures offer effective relief without removing the thyroid.
- Radiofrequency ablation (RFA): Uses heat to selectively destroy enlarged thyroid tissue, gradually reducing the goiter’s size.
- Laser ablation: Targets specific areas of enlarged thyroid tissue with minimal impact on healthy tissue.
- Thyroid artery embolization: Thyroid Artery Embolization blocks the blood flow to the goiter, causing gradual shrinkage over weeks.
These procedures are ideal for patients who cannot undergo surgery or wish to avoid long recovery times. They also maintain thyroid function while relieving pressure-related symptoms such as difficulty swallowing or breathing.
When Surgical Intervention Is Necessary
Surgery is considered for goiters that:
- Cause severe breathing or swallowing difficulty
- Grow rapidly or cause cosmetic concerns
- Show suspicious or potentially malignant features
Partial or total thyroidectomy may be required in these situations. Surgery provides immediate relief of compression symptoms but comes with longer recovery and potential need for lifelong thyroid hormone replacement. Surgical intervention is typically reserved for advanced or high-risk cases.
Follow-Up and Long-Term Monitoring After Treatment
After treatment—surgical or non-surgical—regular follow-up is essential. Ultrasounds monitor thyroid size, and blood tests ensure hormone levels remain stable. Even after successful procedures, gradual monitoring helps detect recurrence, regrowth, or hormonal imbalance early. Patients usually experience improvement over weeks to months, and ongoing care ensures lasting symptom control and preserved thyroid function.
Final Thoughts on Causes and Treatment of Thyroid Goiter
Understanding why thyroid goiter occurs and how it is treated is crucial for safe, effective management. Most goiters are caused by hormonal imbalance, iodine deficiency, structural nodules, or autoimmune conditions. Treatment ranges from monitoring and medication to minimally invasive procedures and surgery when necessary. Early evaluation ensures thyroid function is preserved, reduces the risk of complications, and allows patients to choose the most appropriate management option. With personalized care from an experienced endocrinologist or interventional specialist, thyroid goiter can be managed effectively, safely, and often without surgery.
Frequently Asked Questions About Thyroid Goiter
What causes thyroid goiter most commonly?
Thyroid goiter is most often caused by hormonal imbalance, iodine deficiency, benign nodules, or autoimmune thyroid disorders like Hashimoto’s thyroiditis and Graves’ disease.
Can thyroid goiter be treated without surgery?
Yes, many goiters can be managed with medication, radiofrequency or laser ablation, and thyroid artery embolization, depending on size, symptoms, and hormone levels.
How long does non-surgical goiter treatment take to show results?
Minimally invasive treatments typically reduce goiter size gradually over weeks to months, with follow-up ultrasounds to track progress.
When is thyroid surgery necessary for goiter?
Surgery is usually needed for goiters that compress the airway or esophagus, grow rapidly, or have suspicious or malignant features.
Is thyroid goiter treatment covered by insurance in California?
Many insurance plans cover medically necessary treatments, including non-surgical procedures and surgery, but coverage may vary. Always confirm with your provider.